Article by Levitise: Do Vegetable Seed Oils Cause Faulty Wiring in Your Brain?
6 years ago I wrote a blog post on why I don't like vegetable seed oils and how it looks like that play a role in serious health issues like cancer and heart disease. Since then I have discussed how they contribute to toxicity in your body and how they make you fat.
Have I changed my opinion over the last 6 years? Nope! Actually, I’m doubling down on it.
And today I’m taking a look at it from a brain health point of view. Why? Well, it seems that we are increasingly diagnosing our kids with things like Attention Deficit Disorder (ADD) and Attention-Deficit / Hyperactivity Disorder (ADHD). Indeed, 5% of Singaporean children are diagnosed with ADHD (I wonder how many are undiagnosed). Autism affects 1 in 150 kids in Singapore.

In addition, more and more adults in Singapore are getting Alzheimer’s, Parkinson’s, dementia, and other neuro-degenerative diseases. In a recent research study of 818 participants recruited in Singapore, about half were found to have undiagnosed mild cognitive impairment, a brain condition which indicates the early stages of dementia. Half is a lot!
None of the existing medical solutions seem to help much, and everyone seems to be perplexed as to the root cause of these issues.

I have, in the past, taken a browse through the literature on specific neurodegenerative topics and found a few scientific papers here and there which seem to suggest that too many omega-6 fats can be problematic for brain health. But recently what I did was combine all these under one colloquial umbrella, “Faulty Wiring in the Brain,” and then revisit the literature again.
And there was a lot! I’m going to summarize here in bullets and then provide beefier links in the appendix below.
Scientific Evidence Linking Omega-6 Fats to Brain Health Issues
ADHD
- Children and youth with ADHD have elevated blood ω-6:ω-3 and AA:EPA fatty acid ratios compared to controls.(LaChance et al. 2016)
- High prenatal ω-6:ω-3 ratios preceded subclinical ADHD symptoms during mid-childhood. (López-Vicente et al. 2019)
- Children with ADHD and ASD had low levels of EPA, DHA, and AA, along with high ω-6:ω-3 PUFA ratios, correlating significantly with symptoms. (Parletta et al. 2016)
AUTISM
- A lower prenatal ω-3:ω-6 ratio is associated with more child autistic traits, largely accounted for by higher ω-6 instead of lower ω-3 status. (Steenweg-de Graaff et al. 2016)
- Children with ADHD and ASD had lower DHA, EPA, and AA, higher AA:EPA ratios, and lower ω-3:ω-6 ratios than controls. (Madepalli K. Lakshmana. 2016)
- Maternal diets rich in ω-6 PUFAs during gestation and lactation produce changes in sociability consistent with those observed in ASD, and offspring exposed to such diets had increased anxiety levels. (Jones et al. 2013)
- A change in the ratio of ω-6:ω-3, especially during early life, may induce developmental changes in brain connectivity, synaptogenesis, cognition, and behavior related to ASD. (van Elst et al. 2014)
- Children with autism demonstrated lower red blood cell levels of DHA, EPA, AA, and ω-3:ω-6 ratios. (Joan Jory. 2016)
- Autistic subjects showed a marked reduction in 22:6n-3 (23%), resulting in significantly lower total ω-3 PUFA levels (20%), without significant reduction in the ω-6 PUFA series, leading to a significant increase in the ω-6:ω-3 ratio (25%). (Vancassel et al. 2001)
DEMENTIA
- A review of 14 studies provided evidence supporting an association between the ω-6:ω-3 ratio, cognitive decline, and dementia. (Loef and Walach. 2013)
- Certain dietary patterns with a lower ω-6:3 FA ratio are associated with a reduced risk of cognitive decline. (Andruchow et al. 2017)
ALZHEIMER’S
- Increases in Alzheimer's disease coincide with an increase in the ratio of ω-6 to ω-3 PUFA. (Patterson et al. 2012)
- The ω-3:ω-6 ratio was lower in the Alzheimer's group, and total ω-6 fatty acid levels were higher. (Conquer et al. 2000)
- Regular consumption of ω-6 rich oils without adequate ω-3 intake is associated with an increased risk of dementia and Alzheimer's disease. (Gateau et al. 2007)

Surely, there’s enough smoke here to investigate whether there’s a fire or not? I mean this doesn’t look good.
In summary, the scientific evidence seems to suggest that if you have a high omega-6 to omega-3 ratio (ω-6:ω-3) or just a high amount of omega-6 fats in your brain, then you are more likely to have some sort of faulty wiring in the brain and a disease label.
So why is this happening? Why is this phenomenon increasing? Of course, we could argue that lifespans are increasing so we are living longer, and that allows these issues to develop. But why are brain-related issues not prevalent in centenarian populations such as the Okinawans, Hunza, Abkhasians, Cretans, Sardinians, Nicoyans, etc.? We could also argue that we are overdiagnosing, and that certainly could be the case. But the scientific evidence above should be enough to at least warrant a look at our ancestry and the biochemistry, so let’s take a dive into these.

Our Ancestor’s Omega 6 to Omega 3 Ratio
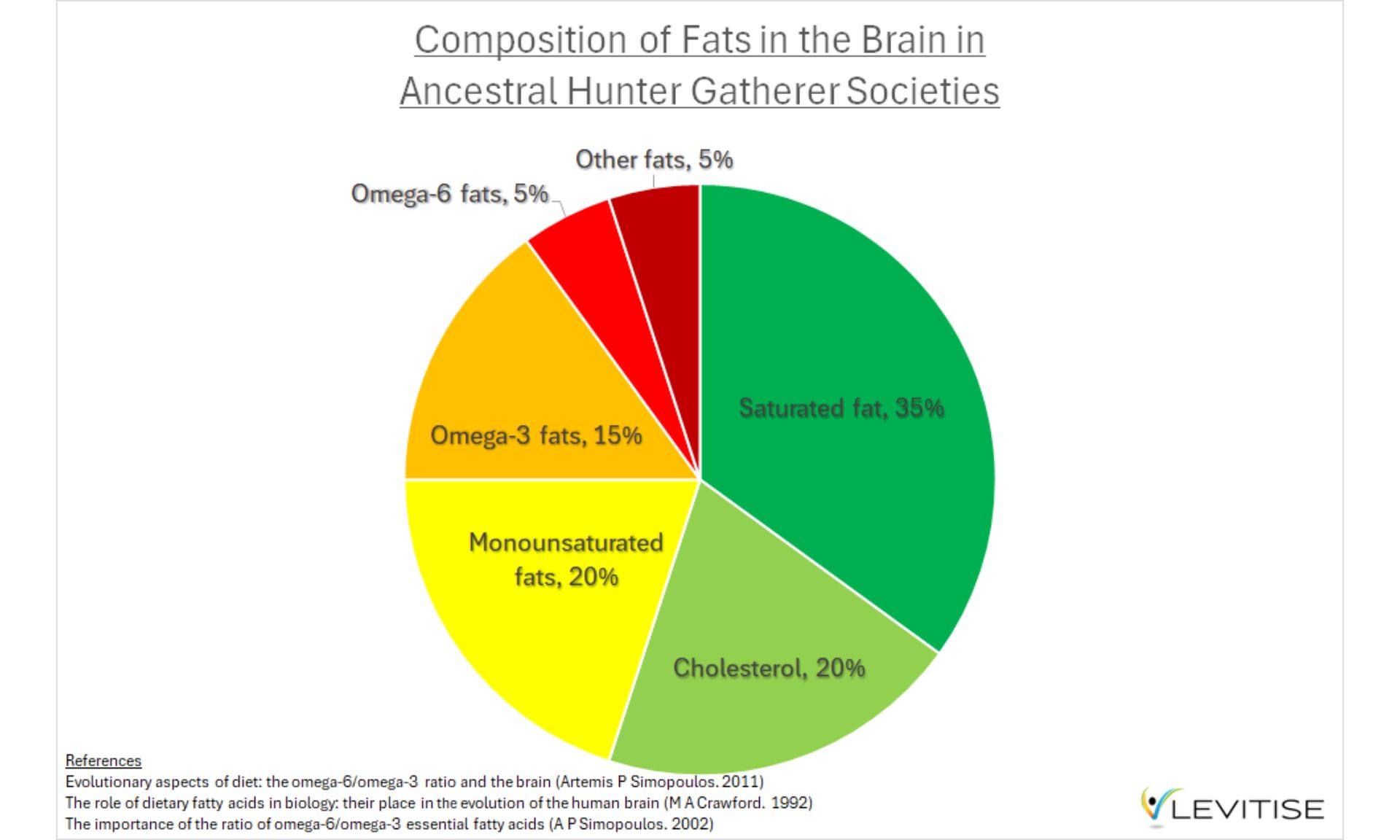
Ancestrally, in hunter-gatherer societies, and early agricultural populations, our landlocked ancestors that thrived on meat tended to have an omega 6:omega 3 ratio of 4:1 whereas our coastal ancestors had an omega 6:omega 3 ratio of only 2:1 (see references below).
The shift in the Western diet, characterized by the increased consumption of processed foods, vegetable oils rich in omega-6 fatty acids (like soybean, corn, and sunflower oils), and a decrease in the consumption of omega-3-rich foods (like fatty fish), has led to a dramatic increase in the omega-6 to omega-3 ratio. In the United States, this ratio is estimated to be around 15:1 to 16.7:1 in the general population, with some estimates suggesting ratios as high as 25:1 or even 50:1 in certain individuals or populations.
Is this modern imbalance contributing to chronic low-grade brain inflammation and neurodegenerative diseases?
Let’s dive a little bit further.
The Biochemistry
I took this straight out of typical medical biochemistry textbooks that first-year medical students would study, such as:
- Lehninger Principles of Biochemistry by David L. Nelson and Michael M. Cox
- Harper's Illustrated Biochemistry by Victor W. Rodwell, David A. Bender, Kathleen M. Botham, Peter J. Kennelly, and P. Anthony Weil
- Biochemistry by Jeremy M. Berg, John L. Tymoczko, and Lubert Stryer
- Medical Biochemistry by John W. Baynes and Marek H. Dominiczak
Inflammatory Response
Omega-6 fatty acids, particularly arachidonic acid (AA), are precursors to pro-inflammatory molecules called prostaglandins, thromboxanes, and leukotrienes. Excessive production of these inflammatory mediators can lead to chronic inflammation in the brain, which is associated with neurodegenerative diseases like Alzheimer's and Parkinson's.
Oxidative Stress
Omega-6 fatty acids are more prone to oxidation compared to omega-3 fatty acids. Oxidative stress occurs when there is an imbalance between the production of reactive oxygen species (ROS) and the body's ability to neutralize them with antioxidants. This oxidative stress can damage brain cells and contribute to neurodegeneration.
Neurotransmitter Function
Omega-3 and omega-6 fatty acids play a role in the structure and function of cell membranes, including those of neurons. Imbalances in the ratio of omega-6 to omega-3 fatty acids can alter membrane fluidity and the function of neurotransmitter receptors, affecting neuronal communication and brain function.
Poor Membrane Fluidity
This can result from an imbalance in omega-6 to omega-3 fatty acids and affect the ability of cells to transport nutrients and waste products across the membrane, leading to cellular toxicity and impaired function.
Neuroinflammation
Neuroinflammation, which is the inflammation of the brain tissue, is associated with neurodegenerative diseases. Excessive omega-6 fatty acids can contribute to neuroinflammation through the production of pro-inflammatory cytokines and other mediators.
Mitochondrial Dysfunction
Mitochondria, the energy-producing organelles in cells, are susceptible to damage from oxidative stress. Excessive omega-6 fatty acids and the resulting oxidative stress can impair mitochondrial function, leading to energy deficits in brain cells and contributing to neurodegeneration.
Synaptic Plasticity
Omega-3 fatty acids, particularly docosahexaenoic acid (DHA), are important for maintaining synaptic plasticity, which is essential for learning and memory. An imbalance in the omega-6 to omega-3 ratio can disrupt synaptic function and contribute to cognitive decline.
That seems pretty conclusive to me. So why is no one talking about his aside from a few fringe players like myself? Why is this topic fringe and not mainstream?
Foods Highest in Omega 6 Fats
I use Cronometer, which has access to the largest nutritional databases in the world. The Gold version has a feature where you can rank your nutrient search by the highest amount of the nutrient per calorie or highest amount per gram. So I plugged in Omega-6 and got the following after removing duplicates.

|
Omega-6 Foods by Highest Amount per Gram |
Per 100g |
| Safflower Oil | 74.62g |
| Grapeseed Oil | 69.60g |
| Sunflower Oil | 65.70g |
| Poppyseed Oil | 62.40g |
| Hemp Oil | 57.35g |
| Vegetable Oil | 56.60g |
| Soybean Oil | 55.68g |
| Wheat Germ Oil | 54.80g |
| Corn Oil | 53.52g |
| Walnut Oil | 52.90g |
To put that into context, a typical 200g grass-fed Aussie steak contains 0.6g of Omega-6 fats, 10g of butter contains 0.1g of omega-6 fats, and a medium-sized egg contains 0.6g. But they all contain saturated fat and cholesterol which will give you a heart attack apparently! I’ve been down that rabbit hole before if you’d like to take a look at those links. And if saturated fat and cholesterol are so bad why did they make up more than 50% of the ancestral brain?
Wrapping Up
Firstly, there appears to be enough scientific evidence to suggest that a diet high in omega-6 fats is bad for our brain health. Secondly, we know that our ancestors had far lower levels of omega-6 fats in our diet than we do now. Whether cavemen children suffered from ADHD or not, or whether the elderly were prone to dementia we’ll probably never know. However, given their diet's composition and the absence of modern-day neurodegenerative diseases, it's plausible that their lower omega-6 intake played a role in their overall brain health. And thirdly, there is plenty of known biochemistry that suggests that consuming too many omega-6 fats promotes neuroinflammation, oxidative stress, mitochondrial dysfunction, and altered neurotransmitter function, all of which contribute to neurodegenerative diseases and poor brain health.
Additionally, something we haven’t explored here is whether our diet, specifically the consumption of vegetable seed oils high in omega-6 fats, is contributing to the rising levels of stress, anxiety, and other aspects of mental wellness in Singapore. It seems logical to me that it would, and this deserves a closer examination as well.
Personally, I avoid this stuff like the plague and don’t feed it to my family. I could be wrong, but even if I am, there’s very little downside.
What do you think?
We’d love your feedback on this article. If you enjoyed it then we’d love to hear from you personally. Just drop us a WhatsApp here and let us know what you liked best about it. Or ask us any questions if you’re not sure. We’re here to help.
To your health, happiness and longevity,
The Levitise Team
Complete References
Palaeolithic nutrition. A consideration of its nature and current implications
(Eaton & Konner. 1985)
Humanity has existed as a genus for about 2 million years, and our prehuman hominid ancestors, the australopithecines, appeared at least 4 million years ago (Table 1). This phase of evolutionary history made definitive contributions to our current genetic composition, partly in response to dietary influences at that time. The foods available to evolving hominids varied widely according to the paleontological period, geographical location, and seasonal conditions, so that our ancestral line maintained the versatility of the omnivore that typifies most primates. Natural selection has provided us with nutritional adaptability; however, human beings today are confronted with diet-related health problems .
https://pubmed.ncbi.nlm.nih.gov/2981409/
Evolutionary aspects of diet, the omega-6/omega-3 ratio and genetic variation: nutritional implications for chronic diseases
Human evolution favored a diet with an omega-6 to omega-3 ratio near 1, but modern Western diets have ratios around 15/1 to 16.7/1, linked to diseases like cardiovascular issues and inflammation. Omega-3s, found in higher levels in the Palaeolithic diet, counter inflammation unlike omega-6s. Genetic variations influence how dietary fats impact health, with a lower omega-6/omega-3 ratio advised for managing chronic diseases, varying based on genetics and disease type.
(A P Simopoulos. 2006)
https://pubmed.ncbi.nlm.nih.gov/17045449/
Omega-6 to Omega-3 Fatty Acid Ratio in Patients with ADHD: A Meta-Analysis
(LaChance et al. 2016)
Children and youth with ADHD have elevated ratios of both blood n6/n3 and AA/EPA fatty acids compared to controls. Thus an elevated n6/n3, and more specifically AA/EPA, ratio may represent the underlying disturbance in essential fatty acid levels in patients with ADHD.
https://pubmed.ncbi.nlm.nih.gov/27274744/
Prenatal Omega-6:Omega-3 Ratio and Attention Deficit and Hyperactivity Disorder Symptoms
(López-Vicente et al. 2019)
High prenatal omega-6:omega-3 long-chain polyunsaturated fatty acid ratio preceded the appearance of subclinical ADHD symptoms during mid-childhood.
https://pubmed.ncbi.nlm.nih.gov/30929929/
Omega-3 and Omega-6 Polyunsaturated Fatty Acid Levels and Correlations with Symptoms in Children with Attention Deficit Hyperactivity Disorder, Autistic Spectrum Disorder and Typically Developing Controls
(Parletta et al. 2016)
Children with ADHD and ASD had low levels of EPA, DHA and AA and high ratio of n-6/n-3 PUFAs and these correlated significantly with symptoms.
https://pubmed.ncbi.nlm.nih.gov/27232999/
Maternal Fatty Acid Status During Pregnancy and Child Autistic Traits: The Generation R Study
(Steenweg-de Graaff et al. 2016)
Our study shows that a lower prenatal ω-3:ω-6 ratio is associated with more child autistic traits, which is largely accounted for by higher ω-6 instead of lower ω-3 status.
https://pubmed.ncbi.nlm.nih.gov/27052119/
Omega-3 and Omega-6 Polyunsaturated Fatty Acid Levels and Correlations with Symptoms in Children with Attention Deficit Hyperactivity Disorder, Autistic Spectrum Disorder and Typically Developing Controls
(Madepalli K. Lakshmana. 2016)
Children with ADHD and ASD had lower DHA, EPA and AA, higher AA/EPA ratio and lower n-3/n-6 than controls. Children with ASD had lower DHA, EPA and AA than children with ADHD.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4883772/
Maternal diet rich in omega-6 polyunsaturated fatty acids during gestation and lactation produces autistic-like sociability deficits in adult offspring
(Jones et al. 2013)
Results indicated that a maternal diet rich in omega-6 PUFAs during gestation and lactation produce changes in sociability consistent with those observed in ASD. Additionally, offspring exposed to a diet rich in omega-6 PUFAs during gestation and lactation had increased levels of anxiety.
https://pubmed.ncbi.nlm.nih.gov/23098794/
Food for thought: dietary changes in essential fatty acid ratios and the increase in autism spectrum disorders
(van Elst et al. 2014)
We argue that a change in the ratio of n-6/n-3, especially during early life, may induce developmental changes in brain connectivity, synaptogenesis, cognition and behaviour that are directly related to ASD.
https://pubmed.ncbi.nlm.nih.gov/25025657/
Abnormal fatty acids in Canadian children with autism
(Joan Jory. 2016)
The children with autism demonstrated lower red blood cell docosahexaenoic acid (P < 0.0003), eicosapentaenoic acid (P < 0.03), arachidonic acid (P < 0.002), and ω-3/ω-6 ratios (P < 0.001).
https://pubmed.ncbi.nlm.nih.gov/26746679/
Plasma fatty acid levels in autistic children
(Vancassel et al. 2001)
Our results showed a marked reduction in the levels of 22: 6n-3 (23%) in the autistic subjects, resulting in significantly lower levels of total (n-3) polyunsaturated fatty acids (PUFA) (20%), without significant reduction in the (n-6) PUFA series, and consequently a significant increase in the (n-6)/(n-3) ratio (25%)
https://pubmed.ncbi.nlm.nih.gov/11487301/
The omega-6/omega-3 ratio and dementia or cognitive decline: a systematic review on human studies and biological evidence
(Loef and Walach. 2013)
Our review of the 14 studies in humans that fulfilled the selection criteria (7 prospective studies, 3 cross-sectional studies, 1 controlled trial, 3 case-control studies) provided evidence supporting an association between the n-6/n-3 ratio, cognitive decline, and incidence of dementia.
https://pubmed.ncbi.nlm.nih.gov/23451843/
A lower ratio of omega-6 to omega-3 fatty acids predicts better hippocampus-dependent spatial memory and cognitive status in older adults
(Andruchow et al. 2017)
In this cross-sectional study, a lower ratio of omega-6 to omega-3 FA intake strongly predicted more accurate hippocampus-dependent spatial memory and faster learning on our virtual navigation tasks, as well as higher cognitive status overall. These results may help elucidate why certain dietary patterns with a lower omega-6:3 FA ratio are associated with reduced risk of cognitive decline.
https://pubmed.ncbi.nlm.nih.gov/28394147/
Oxidized Products of Omega-6 and Omega-3 Long Chain Fatty Acids Are Associated with Increased White Matter Hyperintensity and Poorer Executive Function Performance in a Cohort of Cognitively Normal Hypertensive Older Adults
(Shinto et al. 2020)
Omega-6 derived 9-HODE was associated with increased WMH (p = 0.017) and reduced grey matter volume (p = 0.02). Omega-6 P450-derived diol/epoxide ratio 9,10-DiHOME/9,10-EpOME was associated with increased WMH (p = 0.035) and poorer performance on Trails-B (p = 0.05)
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8597742/
Health implications of high dietary omega-6 polyunsaturated Fatty acids
(Patterson et al. 2012)
Coinciding with this increase in the ratio of (n-6) : (n-3) PUFA are increases in chronic inflammatory diseases such as non-alcoholic fatty liver disease (NAFLD), cardiovascular disease, obesity, inflammatory bowel disease (IBD), rheumatoid arthritis, and Alzheimer's disease (AD).
https://pubmed.ncbi.nlm.nih.gov/22570770/
Fatty acid analysis of blood plasma of patients with Alzheimer's disease, other types of dementia, and cognitive impairment
(Conquer et al. 2000)
In this study we analysed the total phospholipid, phosphatidylcholine (PC), phosphatidylethanolamine (PE), and lysophosphatidylcholine (lysoPC) fractions of plasma from patients diagnosed with AD, OD, or CIND and compared them with a group of elderly control subjects with normal cognitive functioning. Plasma phospholipid and PC levels of 20:5n-3, DHA, total n-3 fatty acids, and the n-3/n-6 ratio were lower in the AD, OD, and CIND groups. Plasma phospholipid 24:0 was lower in the AD, OD, and CIND groups as compared with the group of control patients, and total n-6 fatty acid levels were higher in the AD and CIND groups only.
https://pubmed.ncbi.nlm.nih.gov/11201991/
Dietary patterns and risk of dementia: the Three-City cohort study
(Gateau et al 2007)
Regular consumption of omega-6 rich oils not compensated by consumption of omega-3 rich oils or fish was associated with an increased risk of dementia (HR 2.12, 95% CI 1.30 to 3.46) among ApoE epsilon 4 noncarriers. Increased consumption of n-6 rich oils (sunflower or grape seed oil) was associated with an increased incidence of AD (HR 2.12, 95% CI 1.30 to 3.46) if not counterbalanced by the consumption of n-3 rich food.
